Discussion
I've been on statins for 30-35 yrs or so currently on Avorvastatin 20mg. BMI 22 and 67 years old.
Originally I was put on statins (despite having healthy cholesterol levels) due to T1 diabetes, cholesterol levels have stayed at healthy level, and statin level reduced to where we are now.
A couple of years ago I was diagnosed with heart failure and a reduced LV ejection rate of 27%. Various other meds introduced beta blockers etc.
No sign of heart attack, thickening of arteries etc, angiography all good, heart failure clinic happy, all good. A while afterwards it was recommended I have an internal defibrillator fitted (all done with pace maker turned down to min) due to an unusual momentary atrial fibrillation occurring whilst sleeping.
Recently I've had muscle pains, poor energy levels, poor sleep. As an experiment I stopped taking statinsa few days ago, and started to feel better, not sure if it's coincidence, placebo effect or whatever.
If my cholesterol is in control with a 'sensible T1 diabetic diet' are statins really necessary? The medical profession seem to push them like they're gods gift to health.
Originally I was put on statins (despite having healthy cholesterol levels) due to T1 diabetes, cholesterol levels have stayed at healthy level, and statin level reduced to where we are now.
A couple of years ago I was diagnosed with heart failure and a reduced LV ejection rate of 27%. Various other meds introduced beta blockers etc.
No sign of heart attack, thickening of arteries etc, angiography all good, heart failure clinic happy, all good. A while afterwards it was recommended I have an internal defibrillator fitted (all done with pace maker turned down to min) due to an unusual momentary atrial fibrillation occurring whilst sleeping.
Recently I've had muscle pains, poor energy levels, poor sleep. As an experiment I stopped taking statinsa few days ago, and started to feel better, not sure if it's coincidence, placebo effect or whatever.
If my cholesterol is in control with a 'sensible T1 diabetic diet' are statins really necessary? The medical profession seem to push them like they're gods gift to health.
sensibly all lay people can do is look at the peer reviewd case studies
i found this interesting
https://www1.racgp.org.au/newsgp/clinical/have-the...
i found this interesting
https://www1.racgp.org.au/newsgp/clinical/have-the...
Firstly, if you have a health or medication concern, why not speak to a medical professional who has your record and can examine you, rather than a load of blokes - mainly blokes on a motoring forum?
But then... I was put on statins in 1990 after a heart attack, but was taken off some 3 or 4 years ago. I forget now why.
We are complex and all different.
But then... I was put on statins in 1990 after a heart attack, but was taken off some 3 or 4 years ago. I forget now why.
We are complex and all different.
I was taking 20mg Simvastatin for a few years until I had a heart attack 12 years ago. I was then prescribed Atorvastatin 80mg then the real nightmare began. Frozen shoulder & horrendous muscle pains in my arms.
My Doctor wouldn't have any of it but after doing research I stopped taking statins & surprise surprise the muscle pains stopped. A few years later I agreed to take a low dose statin & was prescribed Simvastatin 30mg. Had no problems since & cholesterol is fine.
Do some research Atorvastatin, muscle pain this problem is widely documented.
My Doctor wouldn't have any of it but after doing research I stopped taking statins & surprise surprise the muscle pains stopped. A few years later I agreed to take a low dose statin & was prescribed Simvastatin 30mg. Had no problems since & cholesterol is fine.
Do some research Atorvastatin, muscle pain this problem is widely documented.
Huzzah said:
I
A couple of years ago I was diagnosed with heart failure and a reduced LV ejection rate of 27%. Various other meds introduced beta blockers etc.
No sign of heart attack, thickening of arteries etc, angiography all good, heart failure clinic happy, all good. A while afterwards it was recommended I have an internal defibrillator fitted (all done with pace maker turned down to min) due to an unusual momentary atrial fibrillation occurring whilst sleeping.
I had a similarly low ejection fraction and it turned out to be a blocked bundle branch - the 'electrical' filaments surrounding the heart that cause it to contract. This was corrected by having something very similar to a pacemaker fitted (which you've had recommended by the sounds of it), which I've had for nearly 10 years. The EF is back to over 50%.A couple of years ago I was diagnosed with heart failure and a reduced LV ejection rate of 27%. Various other meds introduced beta blockers etc.
No sign of heart attack, thickening of arteries etc, angiography all good, heart failure clinic happy, all good. A while afterwards it was recommended I have an internal defibrillator fitted (all done with pace maker turned down to min) due to an unusual momentary atrial fibrillation occurring whilst sleeping.
Happy to answer any questions on a PM if you consider it.
NDA said:
I had a similarly low ejection fraction and it turned out to be a blocked bundle branch - the 'electrical' filaments surrounding the heart that cause it to contract. This was corrected by having something very similar to a pacemaker fitted (which you've had recommended by the sounds of it), which I've had for nearly 10 years. The EF is back to over 50%.
Happy to answer any questions on a PM if you consider it.
Thank you.Happy to answer any questions on a PM if you consider it.
Alickadoo said:
Firstly, if you have a health or medication concern, why not speak to a medical professional who has your record and can examine you, rather than a load of blokes - mainly blokes on a motoring forum?
But then... I was put on statins in 1990 after a heart attack, but was taken off some 3 or 4 years ago. I forget now why.
We are complex and all different.
I generally agree but like to carry out research 1st.But then... I was put on statins in 1990 after a heart attack, but was taken off some 3 or 4 years ago. I forget now why.
We are complex and all different.
GPs and statin use goes something like this.
Elevate cholesterol levels, yup needs statins
Over 50, yup statins a good idea.
Diabetic yup statins required
Heart failure yup stins required
3 out of 4 means it's mandatory!
Anyone know about statin decharge and rechallange.
Edited by Huzzah on Wednesday 20th August 11:41
I'm on max dose Atorvastatin after a STEMI a month ago. I'm no longer taking them for all the reasons you listed in your post, and also the one from gus. GP is mad and has basically said I'm gonna die in 2 seconds.
It's a topic which is impossible to discuss on a platform like this because of vested interests (as has been touched upon). I'm not willing to get into an inevitable argument with the resident GPs over it, but spend some time researching the NHS QOF (Quality and Outcomes Framework) PDF and look at the points awarded to GP Practices for "recommending" certain treatments to patients and the monetary amounts that those points convert to. QOF point bonuses account for between 8 to 20% of a GPs salary. Draw your own conclusions. Don't expect your GP to talk to you or see you again if you decide to stop taking them, unless you agree to take one of their other statins whereby you'll have a prescription written out in approximately 5 seconds.
It's a topic which is impossible to discuss on a platform like this because of vested interests (as has been touched upon). I'm not willing to get into an inevitable argument with the resident GPs over it, but spend some time researching the NHS QOF (Quality and Outcomes Framework) PDF and look at the points awarded to GP Practices for "recommending" certain treatments to patients and the monetary amounts that those points convert to. QOF point bonuses account for between 8 to 20% of a GPs salary. Draw your own conclusions. Don't expect your GP to talk to you or see you again if you decide to stop taking them, unless you agree to take one of their other statins whereby you'll have a prescription written out in approximately 5 seconds.
Tisy said:
I'm on max dose Atorvastatin after a STEMI a month ago. I'm no longer taking them for all the reasons you listed in your post, and also the one from gus. GP is mad and has basically said I'm gonna die in 2 seconds.
It's a topic which is impossible to discuss on a platform like this because of vested interests (as has been touched upon). I'm not willing to get into an inevitable argument with the resident GPs over it, but spend some time researching the NHS QOF (Quality and Outcomes Framework) PDF and look at the points awarded to GP Practices for "recommending" certain treatments to patients and the monetary amounts that those points convert to. QOF point bonuses account for between 8 to 20% of a GPs salary. Draw your own conclusions. Don't expect your GP to talk to you or see you again if you decide to stop taking them, unless you agree to take one of their other statins whereby you'll have a prescription written out in approximately 5 seconds.
Incorrect. By refusing, you are then simply excluded from the QOF indicator so the practice is not affected at all by this. It's a topic which is impossible to discuss on a platform like this because of vested interests (as has been touched upon). I'm not willing to get into an inevitable argument with the resident GPs over it, but spend some time researching the NHS QOF (Quality and Outcomes Framework) PDF and look at the points awarded to GP Practices for "recommending" certain treatments to patients and the monetary amounts that those points convert to. QOF point bonuses account for between 8 to 20% of a GPs salary. Draw your own conclusions. Don't expect your GP to talk to you or see you again if you decide to stop taking them, unless you agree to take one of their other statins whereby you'll have a prescription written out in approximately 5 seconds.
I was put on 20mg atorvastatin daily a few years ago as I had high cholesterol despite a relatively low-fat diet. I soon began to get aches and pains and found this is a fairly common side effect. I asked the GP if there was another statin or similar that I could take without causing muscle pains, but he effectively said "they all do that, sir".
I considered whether I should stop taking the statins but I'm still concerned about the risks of high cholesterol. In the end I compromised by taking one every other day, so effectively halving the dose. I don't get the pains any more, but judging by my annual blood tests it does seem to be still helping a bit with lowering the cholesterol.
I considered whether I should stop taking the statins but I'm still concerned about the risks of high cholesterol. In the end I compromised by taking one every other day, so effectively halving the dose. I don't get the pains any more, but judging by my annual blood tests it does seem to be still helping a bit with lowering the cholesterol.
NDA said:
I had a similarly low ejection fraction and it turned out to be a blocked bundle branch - the 'electrical' filaments surrounding the heart that cause it to contract. This was corrected by having something very similar to a pacemaker fitted (which you've had recommended by the sounds of it), which I've had for nearly 10 years. The EF is back to over 50%.
Happy to answer any questions on a PM if you consider it.
That's a right result, we're you able to come off the beta blocked and stiff?Happy to answer any questions on a PM if you consider it.
Huzzah said:
NDA said:
I had a similarly low ejection fraction and it turned out to be a blocked bundle branch - the 'electrical' filaments surrounding the heart that cause it to contract. This was corrected by having something very similar to a pacemaker fitted (which you've had recommended by the sounds of it), which I've had for nearly 10 years. The EF is back to over 50%.
Happy to answer any questions on a PM if you consider it.
That's a right result, we're you able to come off the beta blocked and stiff?Happy to answer any questions on a PM if you consider it.

I had a heart bypass and some stents too. I am PH's answer to Robocop.
I have taken Statins for over 10 years. With the doctors knowledge and advice I have a pause about every 18 months for a month.
I makes me feel about 10 years younger for that period.
As others have said talk to medical experts first , before you do anything. Ignore all idiots on the internet including me .
I makes me feel about 10 years younger for that period.
As others have said talk to medical experts first , before you do anything. Ignore all idiots on the internet including me .
Granadier said:
I was put on 20mg atorvastatin daily a few years ago as I had high cholesterol despite a relatively low-fat diet. I soon began to get aches and pains and found this is a fairly common side effect. I asked the GP if there was another statin or similar that I could take without causing muscle pains, but he effectively said "they all do that, sir".
I considered whether I should stop taking the statins but I'm still concerned about the risks of high cholesterol. In the end I compromised by taking one every other day, so effectively halving the dose. I don't get the pains any more, but judging by my annual blood tests it does seem to be still helping a bit with lowering the cholesterol.
I stopped taking the statin at night and now take it every morning. My leg muscle pains disappeared within a very short period of time. I considered whether I should stop taking the statins but I'm still concerned about the risks of high cholesterol. In the end I compromised by taking one every other day, so effectively halving the dose. I don't get the pains any more, but judging by my annual blood tests it does seem to be still helping a bit with lowering the cholesterol.
That is interesting what you say about leg paint and statins. I also have leg pain and take statins at night, maybe time to take them in the morning.
I have also got diabetes and my research shows the risks of heart disease and strokes are drastically increased. I have been working on a low carb diet even Thu I am 11stone 3 and 6 foot 1. I am working on the idea that if the blood sugars are good I can reduce the meds with the doctors agreement. This makes sense for type 2 diabetes. The insulin levels are normal but the blood sugars are high, so reducing the sugar input makes more sense than overloading with insulin. We will see how it goes.
I have also got diabetes and my research shows the risks of heart disease and strokes are drastically increased. I have been working on a low carb diet even Thu I am 11stone 3 and 6 foot 1. I am working on the idea that if the blood sugars are good I can reduce the meds with the doctors agreement. This makes sense for type 2 diabetes. The insulin levels are normal but the blood sugars are high, so reducing the sugar input makes more sense than overloading with insulin. We will see how it goes.
Badda said:
Incorrect. By refusing, you are then simply excluded from the QOF indicator so the practice is not affected at all by this.
What percentage of patients would say no to the treatment/management "recommendations" from their GP after being informed that their total cholesterol level is elevated from their recent health check-up and you're at risk of a heart attack? I would bet very few as most people work on the premise that their GP always knows what's best for them and just do what they are told without questioning anything.The total cholesterol is a meaningless number anyway as I'm sure you well know given your occupation, but trying to get a full lipid profile out of a GP for your HDL and non-HDL breakdown is like trying to get blood out of stone. One could make some guesses as to why that is, in light of the financial incentives on offer per the QOF.
Edited by Tisy on Wednesday 20th August 23:43
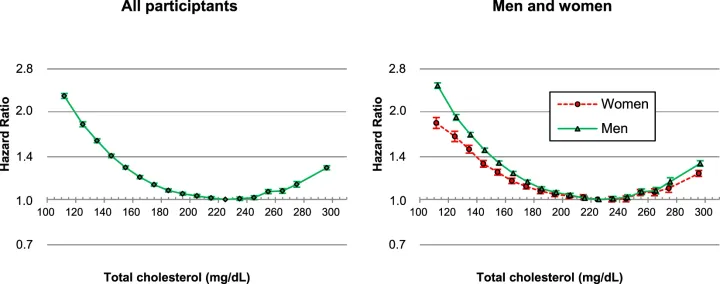
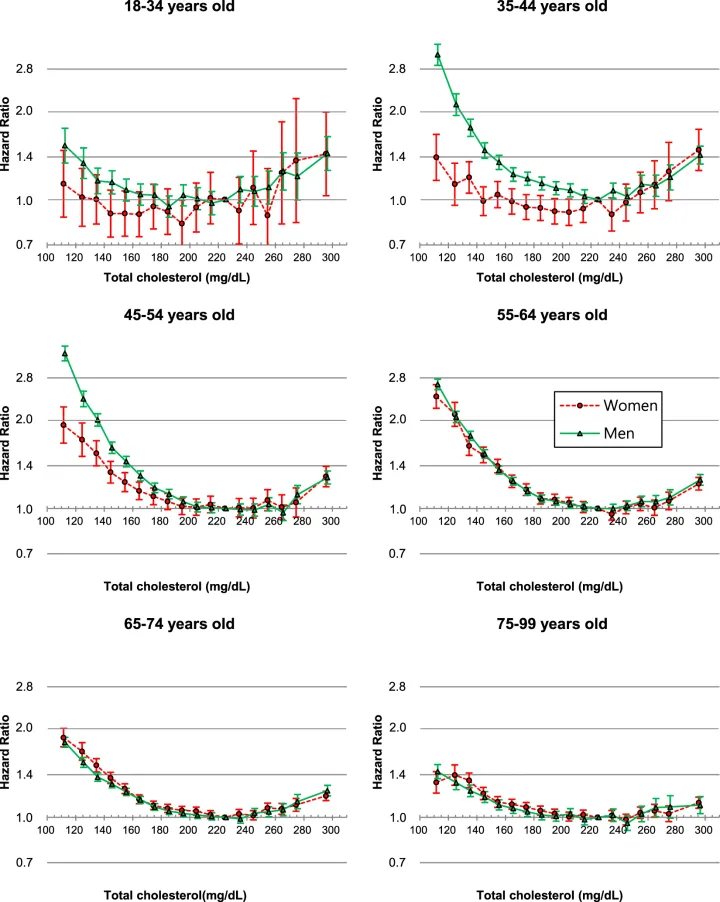
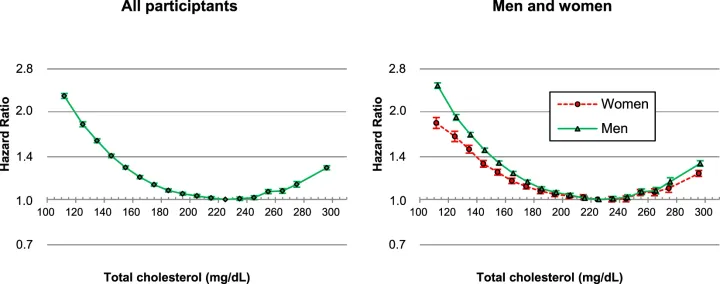
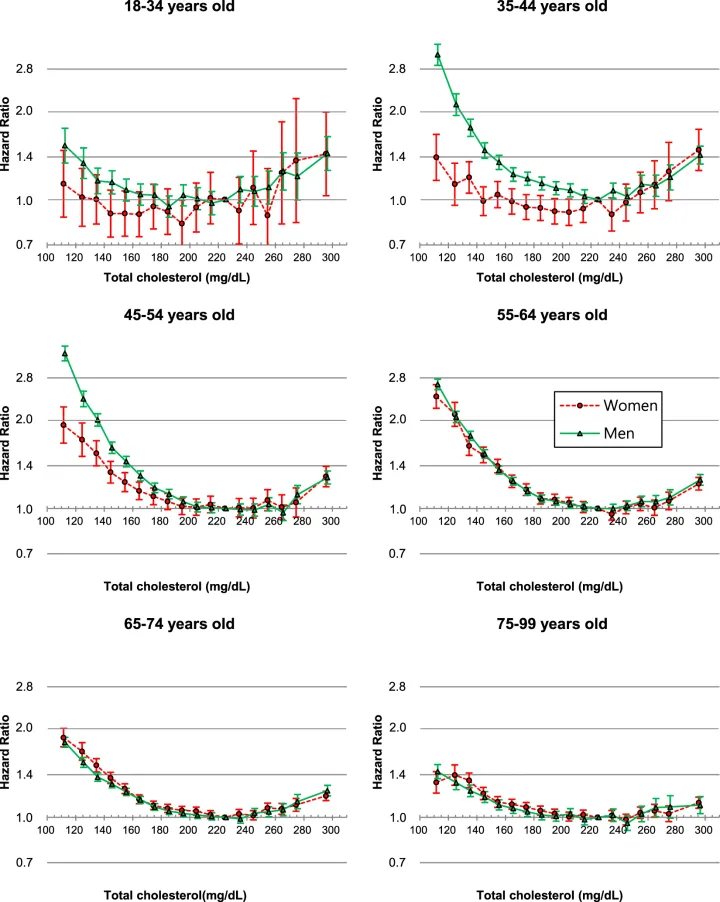
Total cholesterol and all-cause mortality by sex and age: a prospective cohort study among 12.8 million adults
https://www.nature.com/articles/s41598-018-38461-y
Cholesterol is not the problem.
Arterial damage is.
Cholesterol does not cause arterial damage.
https://www.nature.com/articles/s41598-018-38461-y
Cholesterol is not the problem.
Arterial damage is.
Cholesterol does not cause arterial damage.
Tisy said:
Badda said:
Incorrect. By refusing, you are then simply excluded from the QOF indicator so the practice is not affected at all by this.
What percentage of patients would say no to the treatment/management "recommendations" from their GP after being informed that their total cholesterol level is elevated from their recent health check-up and you're at risk of a heart attack? I would bet very few as most people work on the premise that their GP always knows what's best for them and just do what they are told without questioning anything.The total cholesterol is a meaningless number anyway as I'm sure you well know given your occupation, but trying to get a full lipid profile out of a GP for your HDL and non-HDL breakdown is like trying to get blood out of stone. One could make some guesses as to why that is, in light of the financial incentives on offer per the QOF.
Edited by Tisy on Wednesday 20th August 23:43
jagnet said:
Total cholesterol and all-cause mortality by sex and age: a prospective cohort study among 12.8 million adults
https://www.nature.com/articles/s41598-018-38461-y
Cholesterol is not the problem.
Arterial damage is.
Yep, I've got fairly well controlled T2 Diabetes and the danger is that the glucose in the blood damages the artery wall and the small fractional LDL comes along and attempts to repair any damage by forming clots in the artery wall eventually blocking the artery resulting in heart attack/stroke. The only real way to see if you have artery damage is to have a plaque scan (CAC scan) which you can't get on the NHS until you've already had a heart attack, hmmm, surely better to have a scan BEFORE rather than after the event.
Cholesterol does not cause arterial damage.
https://www.nature.com/articles/s41598-018-38461-y
Cholesterol is not the problem.
Arterial damage is.
Yep, I've got fairly well controlled T2 Diabetes and the danger is that the glucose in the blood damages the artery wall and the small fractional LDL comes along and attempts to repair any damage by forming clots in the artery wall eventually blocking the artery resulting in heart attack/stroke. The only real way to see if you have artery damage is to have a plaque scan (CAC scan) which you can't get on the NHS until you've already had a heart attack, hmmm, surely better to have a scan BEFORE rather than after the event.
Cholesterol does not cause arterial damage.
I am on 5mg artovostatin. And have been for I think 7 years.
Until recently I’ve had no side effects and mainly take them for the reduced stroke risk, however the last few months I’ve had a pain in my shoulder, which I put down to poor posture, side sleeping or my work desk set up. But now I wonder if it is made worse by the statins.
Until recently I’ve had no side effects and mainly take them for the reduced stroke risk, however the last few months I’ve had a pain in my shoulder, which I put down to poor posture, side sleeping or my work desk set up. But now I wonder if it is made worse by the statins.
Gassing Station | Health Matters | Top of Page | What's New | My Stuff



